It’s the silent pandemic impacting Australia’s health system and families all over. It’s estimated that every five minutes, an Aussie is diagnosed with diabetes, which is equivalent to almost 300 a day.1
Diabetes is a metabolic and chronic condition where the pancreas can’t produce enough insulin, or, the little insulin it does produce doesn’t work as intended. This results in high blood sugar and other serious complications.
This disease costs our economy $14 billion a year2 and yet is still misunderstood and fraught with confusion.
To coincide with National Diabetes Week, Melanie Clarke, who was diagnosed with the chronic condition almost 20 years ago, shares her story about life with type 1 diabetes, to dispel myths and shed light on this serious condition.
- Diabetes is the seventh most common cause of death by disease in Australia
- 119,000 Aussies live with type 1 diabetes
- 3 million Aussies have type 2 diabetes3
Meet Melanie
Melanie was diagnosed with the chronic condition at nine years old after experiencing mild symptoms, namely extreme thirst. She recalls one particular occasion of having to run out of a yearly exam at school to get water every hour and fearing her teachers would assume she was cheating.
A diabetes diagnosis was furthest from her young mind, although her sister had been diagnosed with it three years earlier.
‘There’s no easy way to tell a child, “you’re going to have to have needles the rest of your life,”’ she said.
The 28-year-old admits her teenage years were particularly difficult, mostly due to the lack of early education on diabetes.
‘I remember having a boyfriend in high school that found out I had diabetes and said, ‘sorry, I don’t want to catch it’. I think that stuck with me; I was always very hesitant to tell anyone for fear they would think I was weird,’ she said. ‘My friends were really good at helping me out when I started to feel low blood sugar. I was always the friend with lollies.’
But today, Melanie describes living with type 1 diabetes as normal. It just so happens that her normal is a bit different than most.

Daily life with type 1 diabetes
Melanie begins every morning with an injection of long and short-acting insulin to ward off any abnormal early-morning increase in blood sugar – not because she ate during the night.
Hormones released in the early part of sleep (called the dawn effect) can increase insulin resistance, causing blood sugar levels to rise.
She also tests her blood glucose levels with a finger pricker regularly and makes small insulin correction injections to keep them within a healthy range of 4–7.8 millimoles per litre of blood (mmol/L) throughout the day. This is especially important to do before meals, so that the insulin can help her body convert glucose (simple sugars from food) into energy quickly, instead of letting it build up in the bloodstream, which can cause complications.
‘When my blood sugar levels get too high, I feel terrible, irritable and thirsty, and almost like my skin is crawling,’ Melanie said.
‘Sometimes when you get sick with the flu, it will go higher as your body is fighting infection and there’s nothing worse. It’s so important to carefully monitor and correct when you’re unwell.’
Melanie sometimes needs up to seven or eight insulin jabs a day, which isn’t without its challenges, especially in her professional life.
‘I’m often working big events with tonnes of people, on my feet for really long days. I can’t always easily just pull out a needle in front of everyone, in fear of freaking them out,’ she said.
Diabetes snapshot
| Type 14 | Type 25 |
| Represents 10% of cases of diabetes | Represents 80-90% of cases of diabetes |
| Usually diagnosed in childhood or adolescence | Often diagnosed in adults over 40 |
| Can be managed only by taking insulin | Can be managed through lifestyle changes and medication |
| Strong hereditary and family-related risk factors | Genetic and lifestyle-related risk factors |
She also exercises regularly but always needs to keep glucose tablets on hand in case her blood sugar levels dip, because intense physical activity causes muscles to use more glucose; this is called hypoglycaemia, otherwise known as the lag effect.
‘I get a bit hesitant doing super physically demanding things for long periods of time because I can almost guarantee my blood sugar will drop low. But hey, diabetics have run marathons, so there’s always a way around it,’ she said.

A happy balance for diet
While diabetes sufferers are usually prescribed strict dietary guidelines to manage their condition, the model and brand ambassador says she doesn’t deprive herself of any foods. Instead, Melanie takes an ‘everything in moderation’ approach. She adjusts her insulin injections accordingly to keep her glucose levels in check. She finds a low-carb diet makes managing diabetes easier, however.
‘Almost all foods have some form of carbohydrate in them. But if I keep my meals under 15 grams, I find it helps keep me more stable, which means fewer injections needed,”’ she said.
According to Melanie, the biggest misconception about diabetes is that it’s linked to poor diet or obesity.
‘I don’t think people realise that type 1 diabetes is actually an autoimmune disease. No one did anything wrong, it’s just your body’s natural reaction and there’s nothing you can do but manage it with insulin,’ she said.
‘People get a shock when I tell them I’m diabetic. I’ve literally been asked, “why aren’t you fat?”’
Despite the lack of education about diabetes and the need for more research to improve outcomes for diabetes sufferers and their families, Melanie has learned to adapt and thrive.
‘We all have ailments; it’s honestly just how you deal with them. I believe that diabetes has lead me to be much more health conscious, and that’s a good thing,’ she said.
More information on diabetes
What’s type 1 diabetes?
Type 1 diabetes is an auto-immune condition where the body attacks and destroys the cells in the pancreas that produce insulin – the hormone the body needs to convert sugar (glucose) from food into energy.
Insulin allows glucose to enter cells to be used as fuel or stored as fat. Without it, the body’s cells can’t absorb glucose. Instead, it just builds up in the bloodstream, which then leads to high blood glucose levels (or hyperglycemia)6 and other health complications.
If the body doesn’t get enough insulin, it begins burning its own fats as energy, which releases chemical substances in the blood acids called ketones. This is a complication called ketoacidosis and can be life-threatening if not treated.7
What’s type 2 diabetes?
Type 2 diabetes is the most prevalent type of diabetes where the body doesn’t produce enough insulin, or the cells stop responding appropriately to insulin and can’t properly absorb glucose for energy. This is known as insulin resistance.
As a result, the pancreas works harder to make more insulin to get glucose into the cells and eventually gets worn out and produces less insulin over time. This causes blood glucose levels to rise too high. That’s why type 2 diabetes is referred to as a progressive condition.
Generally, people who are inactive and overweight or obese have a higher risk of developing type 2 diabetes because extra weight sometimes causes insulin resistance.8
What’s gestational diabetes?
Gestational diabetes only occurs during pregnancy when hormones from the placenta, which help the baby’s development, cause cells to become insulin resistant, leading to higher blood glucose levels.
The condition affects about 12-14% of pregnant women and usually disappears after birth. However, studies suggest that women who develop gestational diabetes have an increased risk of developing type 2 diabetes later in life.9

How do you test for diabetes?
If you suspect you have diabetes or are experiencing symptoms, talk to your general practitioner (GP). Your doctor would usually fill in a pathology request form, which you could take to a pathology collection centre for a blood test.
You can test for diabetes in several ways. These include:
- a glucose test, which doesn’t require fasting and can be done any time in the day;
- a fasting glucose test, which requires you to fast for eight hours (usually overnight) before a blood sample is taken; or
- an oral glucose tolerance test (OGTT), which requires you to fast overnight to have your fasting blood sugar level measured, before drinking a sugary drink and having other blood tests done at one hour and two hours after that.10
It’s important to diagnose diabetes early so that it can be managed and to reduce the risk of complications.
What are diabetes symptoms?
Symptoms of diabetes can range from mild to severe and can occur suddenly or develop gradually in both children and adults. Common diabetes symptoms include:
- extreme thirst
- frequent urination
- tiredness and lethargy
- constant hunger
- slow wound healing
- itching and skin infections
- blurred vision
- unexplained weight loss or gain
- mood swings
- headaches
- dizziness
- leg cramps.11
How can you manage diabetes?
If left untreated, diabetes can cause serious health complications like heart disease and stroke, kidney disease, blindness and limb amputation.
There’s yet no known cure for diabetes, but it can be controlled. Diabetes management aims to keep blood glucose levels as close to ‘normal’, ideally between 4–7.8 millimoles per litre of blood (mmol/L) to reduce the risk of developing serious health complications.
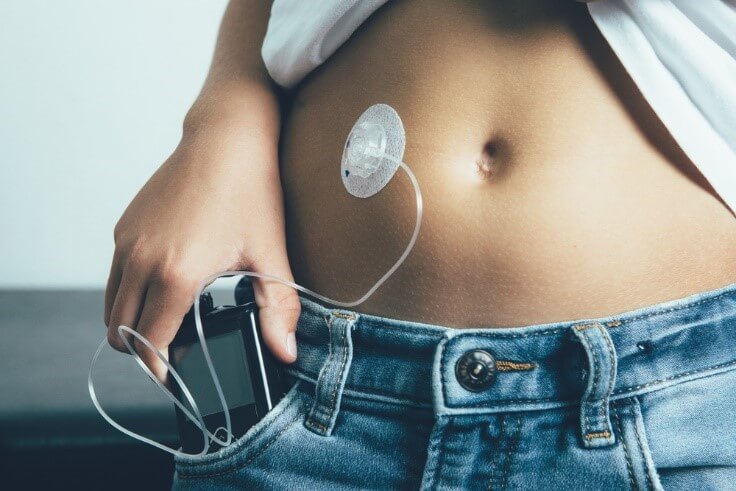
Type 1
Because people who have type 1 diabetes don’t produce insulin naturally, they need daily insulin injections (up to six every day) or an insulin pump (a portable medical device that delivers insulin constantly) to get their insulin, so that their body can absorb glucose and convert it into energy.
Insulin in tablet form doesn’t work as it’s destroyed in the stomach.
Type 1 diabetes sufferers must monitor their blood glucose levels regularly (up to six times per day) and are also usually prescribed a healthy eating plan and exercise routine.12
Exercise especially benefits people with diabetes as it increases insulin sensitivity, which means that the body doesn’t need as much insulin to process glucose.
Type 2
Type 2 diabetes can be managed more easily than type 1, initially through lifestyle changes like following a healthy diet and exercising regularly to help manage blood glucose levels and body weight.
Patients with type 2 diabetes also have to monitor their blood glucose levels regularly to know whether they need to maintain or adjust their treatment.
As type 2 diabetes is a progressive condition, most patients will eventually need medication to help lower their blood glucose levels.13

Does health insurance cover diabetes?
One of the most common ways health insurance can help with the costs associated with diabetes is via coverage towards the cost of insulin pumps, under a Gold hospital tier policy as well as some other tiers Plus policies. The level of coverage you receive will depend on whether the pump is fitted for you as an in-patient (admitted into hospital) hospital procedure or as an out-patient (outside of hospital).
With an appropriate hospital policy, as an impatient, you could be covered towards the cost of your insulin pump prosthesis, as well as your hospital accommodation and doctor’s fees. Most health funds require you to apply for pre-approval before you can claim or receive an insulin pump.
Looking for health insurance?
If you’re considering health insurance to help cover some of the expenses associated with diabetes, our free comparison tool can help you research, compare and buy great health cover- all in the one place. Simply enter a few details, choose your type of cover and what services you want included in your policy and compare.
You can view your options side-by-side from some of Australia’s most reputed health funds. We can help you find great-value cover in just minutes!
Sources
[1] Diabetes Australia- Diabetes in Australia (2019).[2] Diabetes NSW & ACT- Diabetes facts and figures (2019).
[3] Diabetes NSW & ACT- Diabetes facts and figures (2019).
[4] Diabetes Australia- Type 1 diabetes (2019).
[5] Diabetes Australia- Type 2 diabetes (2019).
[6] Mayo Clinic- Hyperglycemia in diabetes (2019).
[7] Victorian Government-Diabetes type 1 (2019).
[8] Diabetes Australia- Type 2 diabetes (2019).
[9] Queensland Government-What is gestational diabetes? (2019).
[10] Mayo Clinic-Diabetes (2019).
[11] Health Direct- Diabetes symptoms (2019).
[12] Diabetes Australia- Managing type 1 (2019).
[12] Diabetes Australia-Managing type 2 (2019).







